by Mehul Gupta, Millie Chau, Megan Howarth et al.
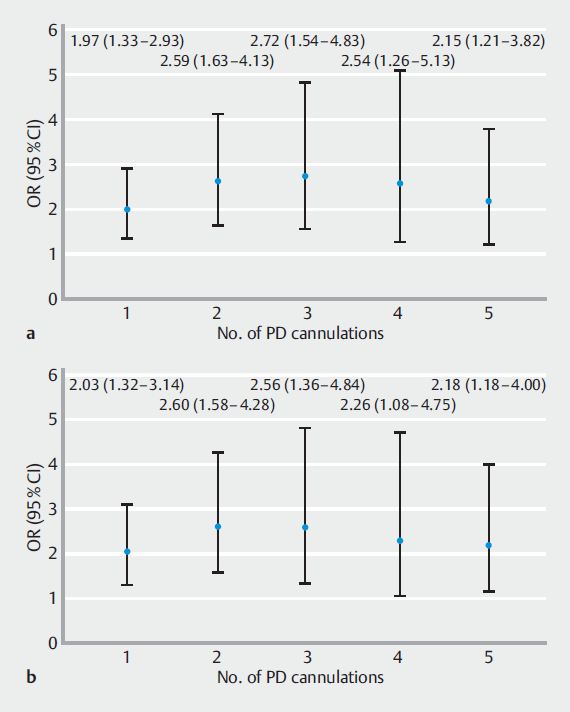
Fig. 1 Relationship between number of main pancreatic duct guidewire cannulations and odds of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis, compared with no pancreatic cannulations. a All patients. b Patients undergoing biliary ERCP for the first time. OR, odds ratio; PD, pancreatic duct.
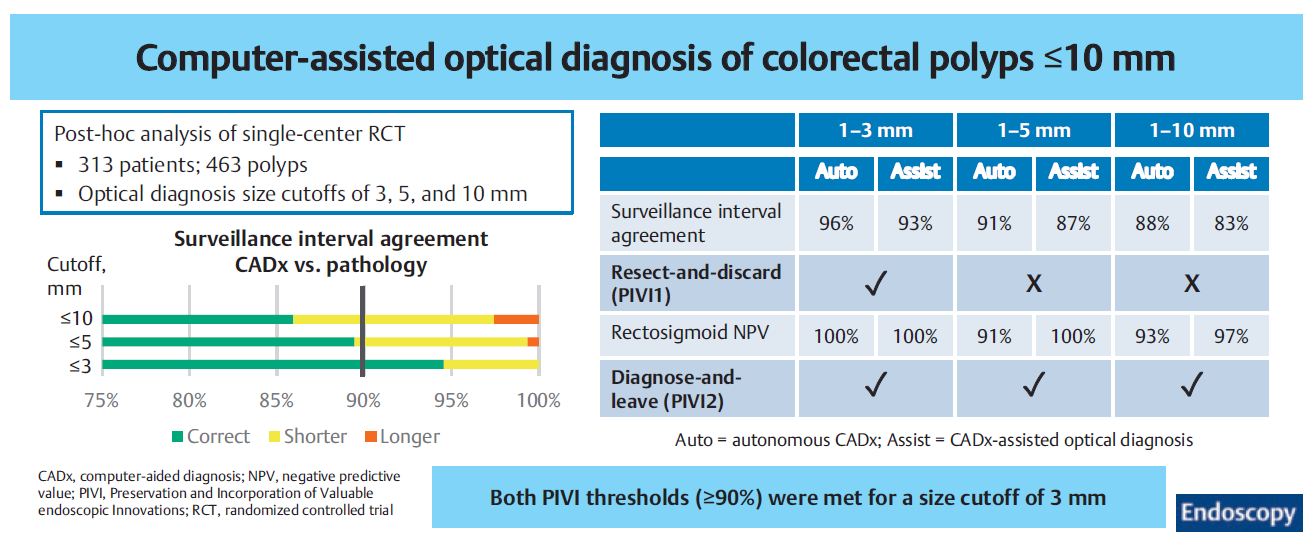
by Megan Oleksiw, Mahsa Taghiakbari, Roupen Djinbachian et al.
by Chi-Liang Cheng, Sergio Cadoni, Paolo Gallittu et al.
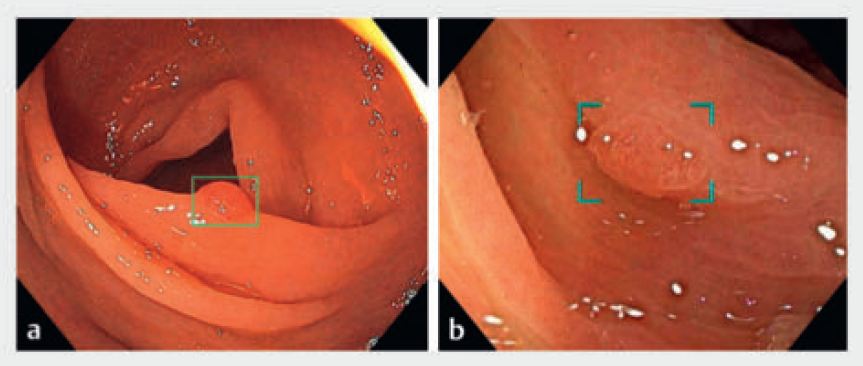
Fig. 1 Images of polyps detected by two computer-aided detection systems. a The ENDO-AID system . b The CAD-EYE system.
by Milou L.M. van Riswijk, Fleur A. Indemans, Kimberly Hawinkels et al.
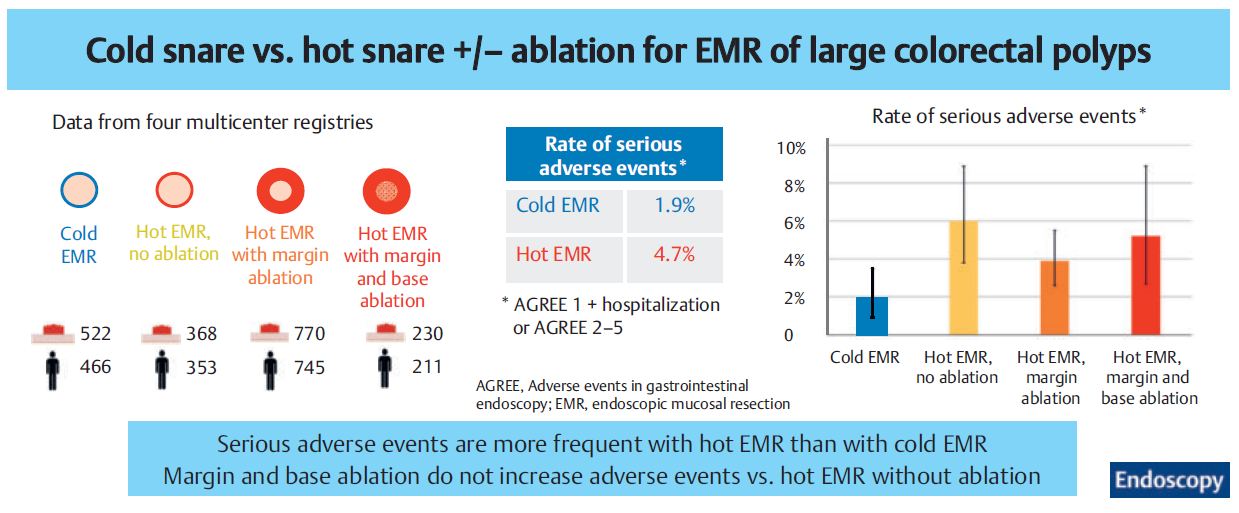
by Edgard Medawar, Heiko Pohl, Douglas K. Rex et al.
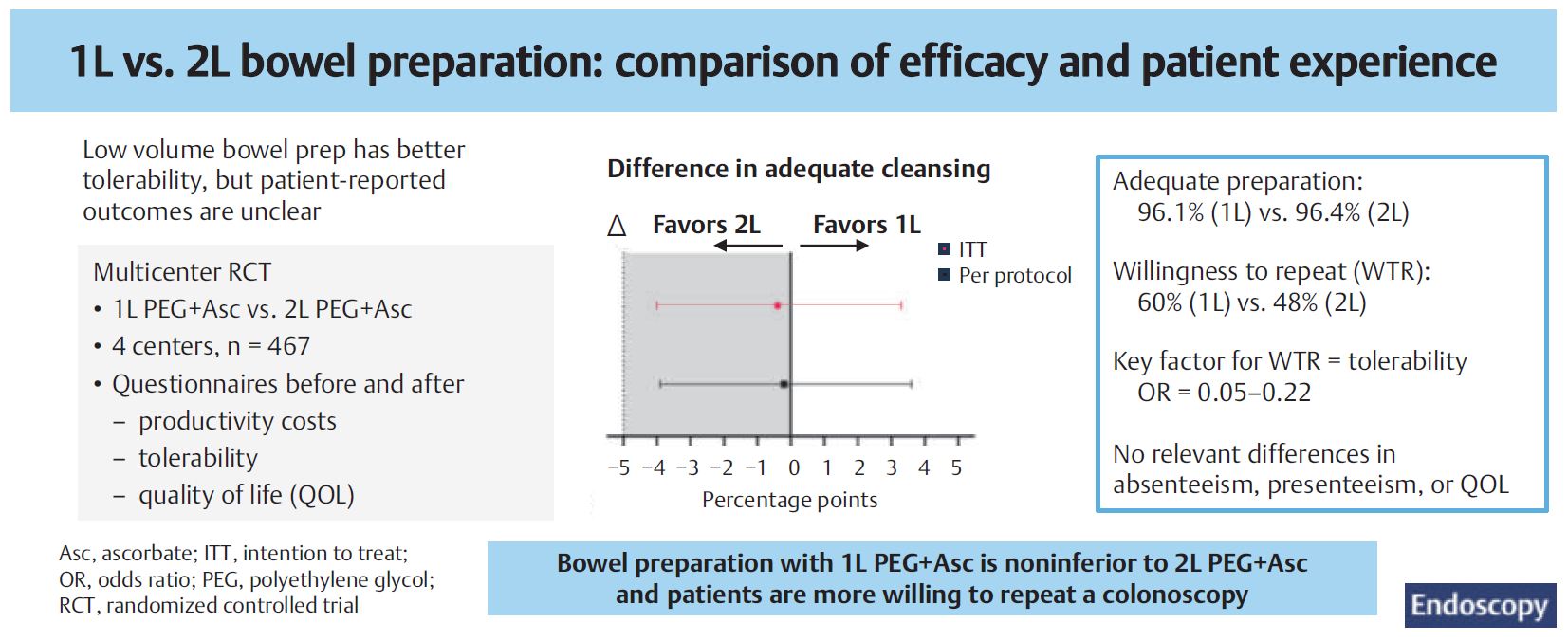
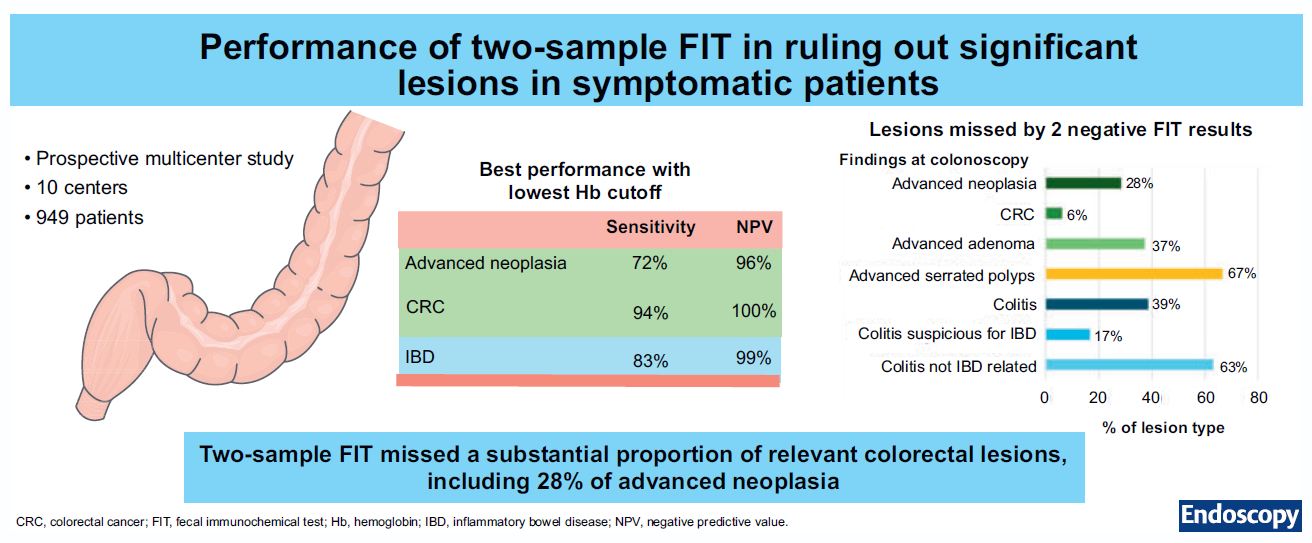
by Sarah Moen, Pieter H.A. Wisse, Fleur Marijnissen et al.
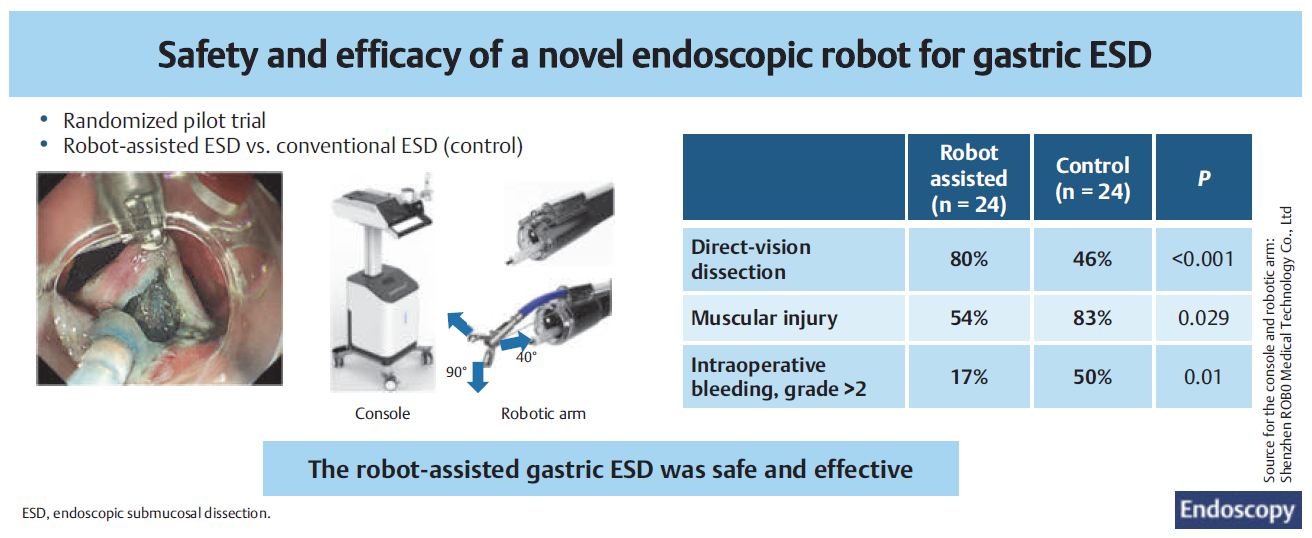
by Ruixin Zhang, Rui Ji, Maosheng Li, Xiaoxiao Yang et al.